Medical Management
Medical Management serves under the direction of the OPNS Chief Medical Officer, Imad Mansoor, M.D., Sandy Foster, RN and the OPNS Quality Assurance/Utilization Management Committee to support our member physicians and provide programs and resources which promote an infrastructure required for success in the ongoing transitions within healthcare delivery.
Medical Management programs support and promote Population Health Management implementation in member physician practices and include:
Quality, Cost and Utilization Management
Medical Management provides quality performance reporting and time sensitive educational resources/training for Health Plan Quality Improvement/Incentive Programs and Cost and Utilization Initiatives including:
• BCBSM Physician Group Incentive Program (PGIP)
• BCBSM Organized System of Care (OSC)
• Blue Care Network (BCN) Commercial HMO Physician Recognition Programs
• BCBSM/BCN Medicare Advantage Physician Recognition Programs
• Priority Health Partners in Performance (PIP) PCP Incentive Program
• Provider Delivered Care Management (PDCM)
• BCBSM Primary Care and Specialist Value-Based Reimbursement (VBR)
• BCBSM Patient Centered Medical Home (PCMH) for PCPs/Neighborhood (PCMH-N) for SPCs
• Pharmacy Cost and Utilization
Care Management
With effective RN Care Management, your practice can improve overall population health, prevent admissions or readmissions and improve the coordination of care for complex patients. In addition, RN Care Management contributes greatly to quality measure improvements, costs of care reductions and patient satisfaction.
RN Care Managers work as part of the Primary Care team, embedded in the office setting. OPNS has developed and successfully implemented this program in 4 Primary Care practices and has added an additional RN Care Manager responsible for managing PDACO beneficiaries discharged to Skilled Nursing Facilities and those discharged home with Home Health Care.
RN Care Management services are currently reimbursed by BCBSM, Priority Health and Medicare.
PCMH/PCMH-N
The PCMH/PCMH-N model drives office workflow to coordinate care between all health care professionals with effective communication, defined roles and responsibilities between providers and patients and supportive interventions in order to better population health management, quality, outcomes and cost. Please visit the PCMH tab on the OPNS website for further details regarding how the PCMH team at OPNS can help facilitate the PCMH model in your practice.
I-MPACT
I-MPACT is a Collaborative Quality Initiative (CQI) that requires hospitals and physician organizations to partner together to improve transitions of care (TOC) in patients with Congestive Heart Failure.
St. Joseph Mercy Oakland and OPNS are working together to improve TOC and reduce avoidable readmissions through these interventions:
• Follow-up phone call within 2 days of discharge
• Follow-up appointment scheduled within 7 days of discharge
End of Life Planning Committee
OPNS established a collaborative End of Life Planning Committee to engage and empower Network physicians and their staff in Advance Care Planning and Palliative Care Services with these goals:
• To assist Network physicians, both PCP and specialists and their care team in engaging patients in discussions of goals, preferences and priorities for end of life care
• To achieve measurable improvement in advance care planning through the development and implementation of standardized processes for engaging patients in Advance Care Planning conversations, and the execution and documentation of a Patient Advocate and Advance Directive forms in these patients’ medical records
• To promote awareness of providing earlier supportive Palliative/Hospice care services
• To provide resources and interventions to address advance care planning
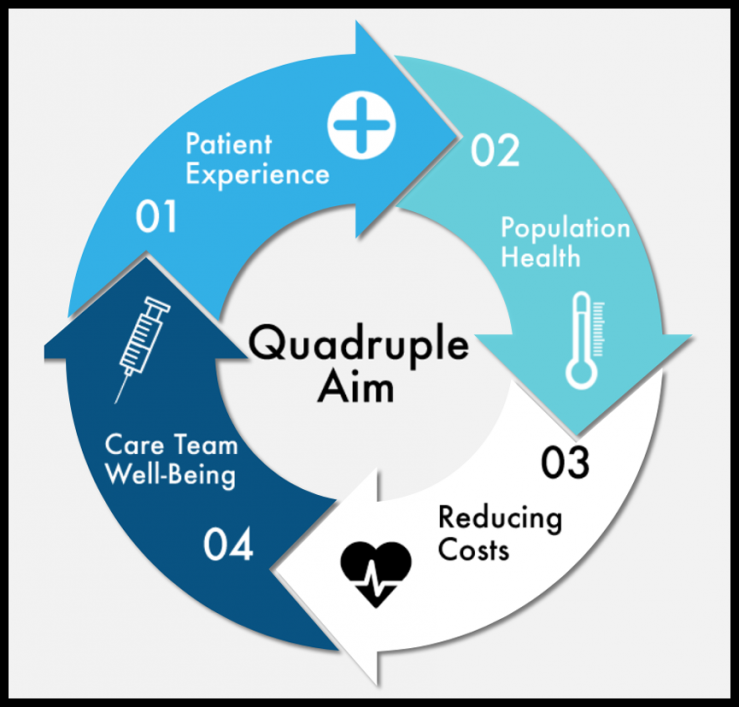
Medical Management supports Network physician practices in the transformation of healthcare delivery processes and promotes the Institute for Healthcare Improvement (IHI) “Triple Aim” Initiative.
Active engagement in Quality Improvement programs as well as the implementation of Healthcare Information Technology products supported by OPNS are critical to the continued success of OPNS and its member physicians.
